On some occasions sponsors and investigators might challenge the need to collect concomitant medications during clinical trials. In this article, we briefly summarize the importance and the most extended good practices for collecting concomitant medications.
The collection of concomitant medications together with safety and efficacy data is of major importance to assess potential drug interactions. Drug interactions between new medical products and marketed drugs must be investigated during clinical development. Drug interactions might be the cause of adverse reactions and affect efficacy by diminishing or even eliminating its effect. These interactions are systematically assessed by pharmacokinetic and pharmacodynamic studies conducted in vitro or in vivo during early stages of clinical development as described in the CHMP Guideline on the investigation of drug interactions. [1]
Although in most cases potential drug interactions are well defined before reaching phase II or phase III clinical trials, it will be important to collect information about possible drug interaction during all phases. For this reason, it will be required the collection of any concomitant treatments like drugs or biological products. In some instances, the collection of food supplements or even food intake might be of interest to evaluate interactions with the investigational drug.
Collection of concomitant medications
The Guidelines for Good Clinical Practices [2] states that all concomitants medications must be reported in accordance with the protocol on the CRFs and that the study protocol must include the concomitant treatments permitted and not permitted before and/or during the trial.
The Clinical Data Acquisition Standards Harmonization (CDASH) defines a minimal data collection set for concomitant medications among other sixteen safety data domains, harmonizing element names, definitions and metadata [3]. Concomitant medications are usually collected by the commercial name within the Case Report Form (CRF). Commercial names are later standardized using generic names as defined in dictionaries like WHO Drug, or WHOCC-ATC Index. An example of a CRF section based on these recommendations developed in Openclinica can be found here. This CRF section allows the collection of concomitant medications facilitating the codification of terms by suggesting generic names. The Excel file for the implementation of this CRF in Openclinica is also available under request.
Data review and validation
Clinical data validation should also include the review of concomitant medications. Current Electronic Data Capture systems like Openclinica or Oracle Inform can help to automatize this process by assessing in real time completeness and consistency with other variables within the CRF. Consistency assessments between concomitant medications and their linked indications might be difficult to evaluate by automatic processes. In these cases, Clinical Research Associates (CRAs) during clinical monitoring visits, or medical monitors during safety data reviews will have important roles for data validation and consistency review.
Reporting
The expected content for a Clinical Study Report (CSR) is described in the guideline ICH E3 Structure and content of clinical study reports. The guideline states the importance about discussing how allowed concomitant therapies might affect the study outcome due either to drug-drug interaction or to direct effects on the study endpoints. [4]
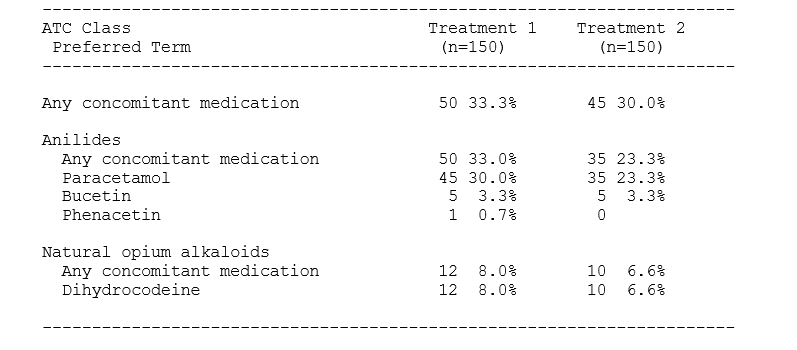
Concomitant medications are usually summarized separately by ATC Class and Preferred Term indicating the number of subjects and percentage. When calculating the use of concomitant medications, each subject is counted only once, and any repetitions of medications are usually ignored; i.e., the denominator corresponds to the total number of subjects. The following table presents a standard output layout to summarize concomitant medications:
Conclusion
Concomitant medications could include drugs, biological products and even food supplements that a study participant takes along with the study medication. Concomitant medications are collected to evaluate potential interactions with the study medication in terms of safety and efficacy. The requirements for recording concomitant medications should be specified in the study protocol.
Autors: Juan V. Torres (Syntax CEO), Lidia Almirall (Syntax COO) María José Estefano (Syntax QAM), Marina Llopis (Syntax DM) and César García-Rey (Syntax CMO).
References
[1] Guideline on the investigation of drug interactions. Committee for Human Medicinal Products (CHMP). CPMP/EWP/560/95/Rev. 1 Corr. 2. 2012.
[2] Guideline for Good Clinical Practice. ICH-E6 (R2)
[3] Clinical Data Acquisition Standards Harmonization (CDASH). CDISC CDASH Team. Version 1.1, 2011.
[4] ICH E3 Structure and content of clinical study reports. CPMP/ICH/137/95, 1996.